What Healthcare Providers Need to Know About Cerebral Perfusion and Treatment-Resistant Depression
As healthcare providers, we’ve long understood that major depressive disorder is a multifactorial illness involving neurotransmitters, psychosocial elements, and often a complex web of life experiences. But what happens when standard interventions fall short? What if we're missing a critical physiological factor—one that isn’t always part of traditional psychiatric evaluation?
This article examines the case of a patient with refractory bipolar depression who failed to respond to the conventional algorithm over two years. It explores the role of cerebral perfusion in treatment-resistant depression (TRD) and presents compelling data on how integrated imaging and treatment strategies, particularly the combination of transcranial magnetic stimulation (TMS) and ketamine, may offer new hope for patients who haven’t responded to conventional care.
Why treatment-resistant depression requires a deeper look
Many of us encounter patients who, despite multiple medication trials, psychotherapy, and even lifestyle modification, continue to suffer. Treatment-resistant depression accounts for a significant proportion of these cases, and its toll is profound—from functional disability to increased risk of suicide.
One emerging hypothesis is that compromised cerebral perfusion may be a contributing factor in TRD. Brain regions with suboptimal blood flow may underperform, regardless of neurochemical modulation. Identifying and addressing this perfusion deficit may be the key to improving outcomes in select patients.
Imaging perfusion with SPECT scans
Single Photon Emission Computed Tomography (SPECT) provides a window into cerebral perfusion, revealing areas of the brain that may not be functioning at full capacity due to hypoperfusion. Unlike structural imaging, SPECT allows us to assess function and activity in real time.
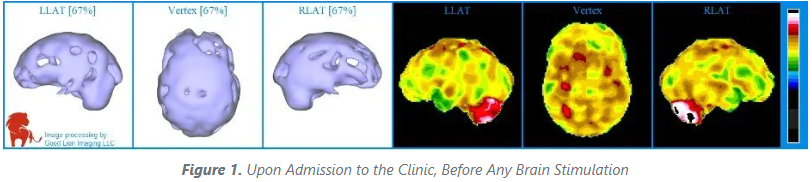
In the clinical case described, Figure 1 illustrates a baseline SPECT scan with widespread hypoperfusion. These darkened areas suggest poor metabolic activity across large swaths of cortex, particularly in regions associated with executive function and mood regulation.
An axial view from the top of the head, underscores the severity of perfusion deficits in prefrontal and temporal lobes—regions implicated in both cognition and emotional processing. The value of this imaging lies in its ability to tailor treatment approaches to each patient’s unique brain activity map.
Integrating TMS and ketamine: a synergistic approach
With perfusion insights in hand, the next question becomes: how do we target these underactive regions? This is where the combination of TMS and ketamine shows promise.
TMS, particularly low-frequency (1 Hz) right-sided stimulation, has been associated with increased regional cerebral blood flow. In practice, this means we can help "wake up" areas of the brain that are quiet due to poor perfusion, without systemic side effects.
Ketamine, a well-established NMDA receptor antagonist, has rapid antidepressant effects. It promotes synaptogenesis and enhances neuroplasticity, particularly when administered in a sub-anesthetic dose.
When paired, TMS primes the brain through increased circulation, while ketamine fosters the development of new synaptic pathways. This dual mechanism is especially useful in patients with refractory depression, where neither treatment alone may be sufficient.
Real-world application and outcomes
At The Neuroscience Center, we’ve implemented this combined protocol with over 85% of patients showing significant clinical improvement. In the case described earlier, a follow-up scan (Figure 2) taken after clinical recovery showed clear perfusion improvements. Patients described more stable mood, increased energy, and even cognitive clarity—outcomes that had eluded them for years.
This evidence suggests that not only are these patients responding subjectively, but their neurophysiology is measurably changing. For referring providers, this presents a viable next step when standard pathways have failed.
When and why to refer
Consider referring to a clinic with access to SPECT imaging and integrated treatment protocols when:
Your patient has not responded to two or more antidepressants.
There is functional decline impacting work or relationships.
The patient expresses frustration with conventional approaches.
There are comorbidities, such as anxiety or cognitive issues, that complicate treatment.
Clinics using perfusion imaging can offer not only targeted interventions but also a clearer picture of what your patient is experiencing neurologically. This enhances shared decision-making and empowers patients to take the next step with confidence.
Final thoughts
As mental health care evolves, our tools must evolve with it. For some patients, depression is not just a psychological or biochemical issue, it may also be a physiological one involving blood flow.
Functional imaging and integrated therapies like TMS and ketamine, guided by perfusion data, represent the future of personalized mental health care. For clinicians navigating the complexities of TRD, these approaches provide both insight and actionable solutions.
If you would like to explore a referral or learn more about this treatment model, here at The Neuroscience Center we’re happy to provide additional information or collaborate on care.
For more information contact: schedule@neuroscience.md
Dr Best is the director of The Neuroscience Center in Deerfield, Illinois. Dr Pavel was the director of PathFinder Brain SPECT, and a professor of radiology and nuclear medicine at the University of Illinois Medical Center. This article is published posthumously; Dr Pavel passed away in 2021.
To read the original published case study by Dr. Best and Dr. Pavel, visit What’s Perfusion Got to Do With It? at Psychiatric Times.