Depression and the Delivery Problem No One Talks About
Imagine your brain as a thriving, high-tech city. The neurons are busy residents sending messages, the electrical signals are the high-speed internet lines keeping everyone connected, and blood flow? That’s the logistics network, delivering everything from oxygen and nutrients to essential messengers that keep things running smoothly.
Now imagine there’s a bottleneck. Deliveries get delayed, neighborhoods start to struggle, and even small issues become big problems. That’s what happens in the brain when perfusion—meaning blood flow—is compromised. And in one patient’s story, this proved to be a missing link in why their severe depression wouldn’t budge, no matter how many treatments they tried.
Why traditional depression treatment doesn’t always work
We’ve known for a while that blood flow in the brain plays a major role in cognition, memory, and emotional regulation. But now we’re seeing more clearly how it connects to mental health treatment outcomes, too.
In the case described here, a patient with severe bipolar depression had spent over two years trying standard treatments without success. What if the core issue wasn’t just about mood chemicals or past trauma, but something more physical—like specific parts of their brain simply not getting enough blood to function properly?
We’ve long known that blood flow in the brain plays a role in things like thinking, memory, and emotion. But we’re now understanding that it may also help explain why some people don’t respond to traditional mental health treatments.
How imaging reveals what’s really going on
To investigate blood flow in the brain, physicians can use a type of scan called SPECT (Single Photon Emission Computed Tomography). It lets them observe how different regions of the brain are being perfused—or not.
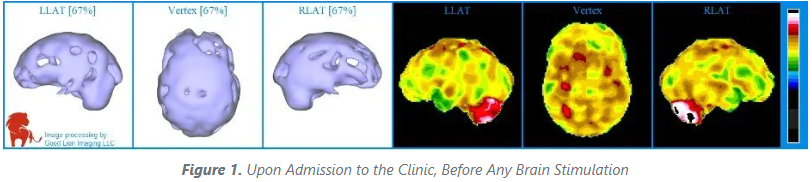
In this patient’s baseline SPECT scan (Figure 1), large areas of the brain showed reduced perfusion. It looked like parts of the city had lost power. Viewed from the top of the head, the images revealed that brain regions involved in mood and decision-making weren’t getting the blood supply they needed.
This kind of insight allowed us to tailor a more targeted, science-based treatment approach.
A one-two punch: combining TMS and ketamine
Enter two promising therapies: transcranial magnetic stimulation (TMS) and ketamine. Both have made a name for themselves in the treatment of resistant depression. But when used together, their impact may be even greater.
Let’s break it down:
TMS uses magnetic pulses applied to the scalp to stimulate areas of the brain that are underactive. In this case, a low frequency (1 pulse per second) was used. This frequency has been shown to increase blood flow in targeted areas. Think of it like jump-starting parts of the brain that have gone quiet due to poor circulation.
Ketamine, on the other hand, is a powerful anesthetic that, in low doses, can act as a fast-acting antidepressant. It works by encouraging the brain to form new connections and improve its adaptability.
When used together, TMS enhances circulation, and ketamine boosts the brain’s capacity to rebuild. It’s like fixing the roads and expanding the train system. The result? A faster, more reliable recovery from depression.
Real-world results that matter
After this combined treatment, the patient experienced a dramatic turnaround. In fact, over 85% of patients treated at The Neuroscience Center using this approach have reported significant improvement. In this case, the patient saw better mood, energy, and focus after several sessions.
A follow-up scan (Figure 2) revealed a clear increase in blood flow to the previously underactive areas of the brain.
For patients, this isn’t just about a better scan. It’s about energy returning, mood stabilizing, and hope being restored.
Why this matters for patients and families
If you or someone you love has been living with depression that doesn’t seem to budge, it’s important to know that there are emerging, science-based treatments that go beyond traditional medications.
Looking at the brain’s blood flow—literally how well it's being “fed”—offers a new lens for treatment. By using imaging to guide therapy and combining interventions in smarter ways, we’re getting closer to unlocking better mental health outcomes for more people.
This is about meeting the brain where it’s struggling, and giving it what it needs to heal.
The bottom line: blood flow is more than just biology
Your brain is a miracle of biology and engineering. It's not only about neurotransmitters and psychology—it’s also about oxygen, circulation, energy, and coordinated network functions. When parts of the brain aren’t getting the blood they need, they can’t perform at their best.
But now, with advanced tools like SPECT imaging and the thoughtful use of treatments like the combination therapy of TMS and ketamine, we can do something about it.
So yes, when it comes to depression, blood flow has everything to do with it.
If you or a loved one is struggling with depression that hasn’t improved with traditional treatment, we’re here to help. Reach out to The Neuroscience Center to learn more about how advanced imaging and innovative therapies like TMS and ketamine could be the next step toward recovery. Your journey matters—and you don’t have to walk it alone.
Dr Best is the director of The Neuroscience Center in Deerfield, Illinois. Dr Pavel was the director of PathFinder Brain SPECT, and a professor of radiology and nuclear medicine at the University of Illinois Medical Center. This article is published posthumously; Dr Pavel passed away in 2021.
To read the original published case study by Dr. Best and Dr. Pavel, visit What’s Perfusion Got to Do With It? at Psychiatric Times.